Link between PCOS And Diabetes
Polycystic Ovary Syndrome (PCOS) and Diabetes are two conditions that are commonly seen in women of reproductive age and both are related to hormonal imbalances. In recent years, research has shown that there may be a strong link between PCOS and Diabetes.
In this article, we will look at how these two things are related to each other in detail so that you gain a better understanding.
What is PCOS?
A hormonal condition known as polycystic ovary syndrome (PCOS) affects many women of reproductive age. Cysts in the ovaries, irregular menstrual cycles, and high amounts of androgens (male hormones) are its defining characteristics. These factors can cause symptoms like acne, excessive hair growth, and weight gain. In addition to affecting fertility, PCOS raises the chance of developing certain illnesses like type 2 diabetes and heart disease.
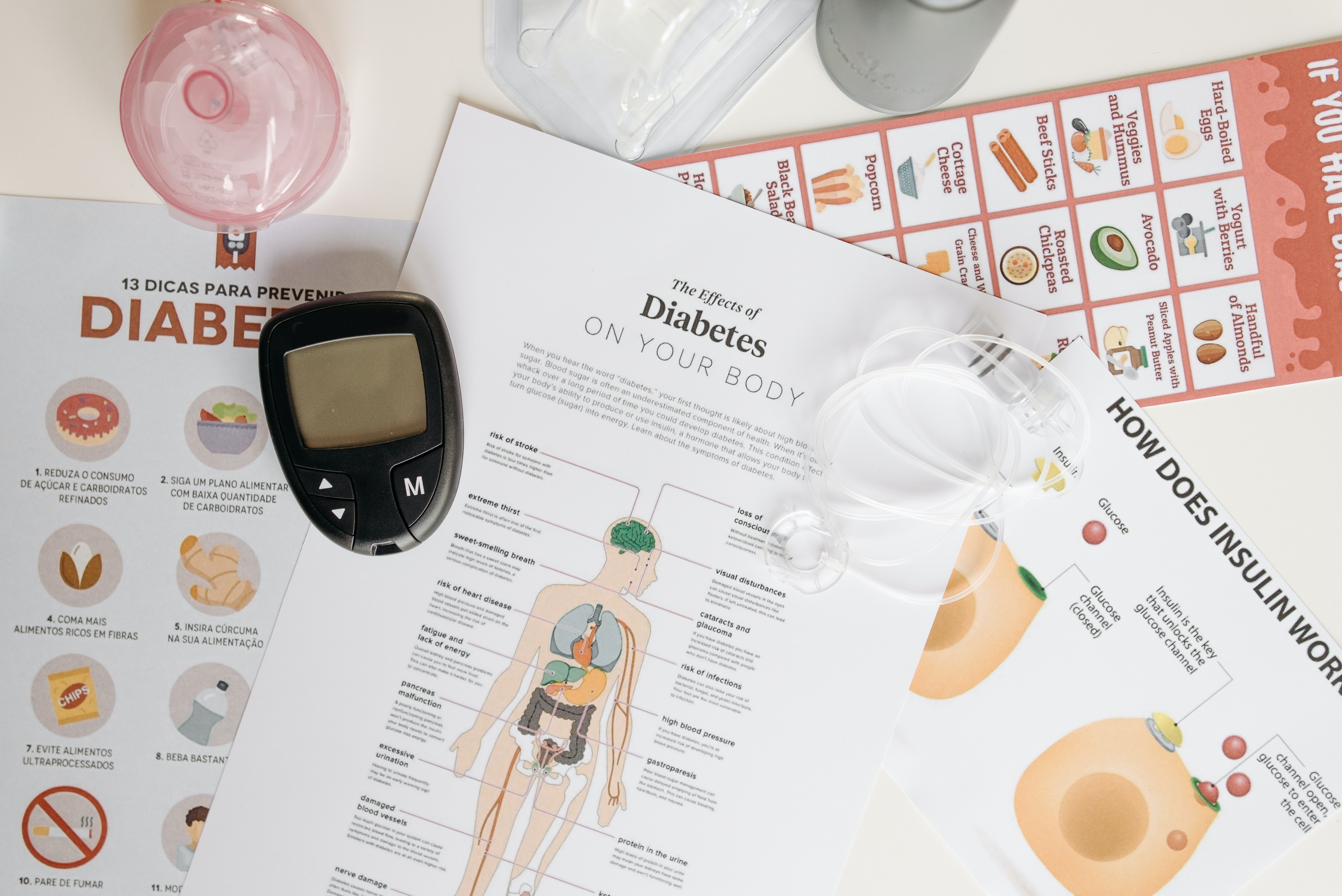
What are diabetes and its type?
Diabetes occurs when there is an issue with the hormone insulin and the way it regulates glucose (sugar) in the body. In a healthy individual, insulin helps move glucose from the blood into the cells where it is used for energy. However, in diabetes, this process is disrupted.
Type 1 diabetes is an autoimmune disorder where the body's immune system mistakenly attacks and destroys the cells in the pancreas that produce insulin. As a result, the body is unable to produce insulin and must rely on injections or insulin pumps to regulate blood sugar levels.
Type 2 diabetes is a metabolic disorder that occurs when the body becomes resistant to insulin or doesn't produce enough insulin to regulate blood sugar levels effectively. This can be due to a combination of genetic and environmental factors, such as an unhealthy diet, lack of physical activity, and being overweight or obese.
Both types of diabetes can lead to elevated levels of glucose in the blood, which can damage blood vessels, nerves, and organs if left uncontrolled.

How are Diabetes and PCOS related?
Polycystic ovary syndrome (PCOS) is a hormonal disorder common among women of reproductive age that can impact their menstrual cycle, fertility, and insulin metabolism.
Women with PCOS often have insulin resistance. Insulin resistance in PCOS is a condition where the cells in the body become less sensitive to insulin. As a result, more insulin is needed to move glucose into cells, leading to higher levels of insulin in the bloodstream.
In women with PCOS, insulin resistance can be caused by a number of factors, including hormonal imbalances, increased levels of androgens (male hormones), and excess weight.
This insulin resistance can contribute to the symptoms of PCOS, such as irregular periods, ovary enlargement, and excess hair growth. Additionally, it can increase the risk of developing type 2 diabetes and cardiovascular disease.
Additionally, women with PCOS have an increased risk of obesity, which can also contribute to the development of type 2 diabetes.
How Can Insulin Resistance in Women with PCOS Be Treated?
Insulin resistance in women with PCOS can be treated with a combination of lifestyle changes and medications. Here are some common treatments:
Lifestyle changes
Eating a balanced diet with plenty of fibre and healthy fats, along with regular physical activity, can help improve insulin sensitivity and regulate blood sugar levels.
Weight loss
Women with PCOS who are overweight or obese may benefit from losing weight. Weight loss can help improve insulin sensitivity and reduce the symptoms of PCOS.
Metformin
This is a medication that helps improve insulin sensitivity and lower blood sugar levels. It can also help regulate menstrual cycles and improve fertility in women with PCOS.
Ovarian suppression
Hormonal therapy using birth control pills or other medications can suppress ovulation and reduce the production of androgens, which can improve insulin sensitivity and reduce symptoms of PCOS.
Thiazolidinediones (TZDs)
These medications can improve insulin sensitivity and help lower blood sugar levels.
Liraglutide
This is a glucagon-like peptide-1 (GLP-1) receptor agonist that has been shown to help improve insulin sensitivity and weight loss in women with PCOS.
It's important to work with a doctor to determine the best treatment plan for insulin resistance in PCOS, as each woman's situation is unique. Lifestyle changes and medications can be effective in managing insulin resistance and improving overall health in women with PCOS.
Frequently Asked Questions
We know that you might have a lot of questions about PCOS and its relation with diabetes, which is why we have compiled a list of frequently asked questions for you, have a look-
Can diabetes be a cause of PCOS?
No, diabetes does not directly lead to Polycystic Ovary Syndrome (PCOS). However, women with PCOS have an increased risk of developing type 2 diabetes, and women with type 2 diabetes have an increased risk of developing PCOS.
What is similar between diabetes and PCOS?
Both Diabetes and Polycystic Ovary Syndrome (PCOS) are related to hormonal imbalances and are associated with insulin resistance. In both conditions, the body has difficulty using insulin effectively, leading to elevated blood sugar levels. Additionally, both Diabetes and PCOS can lead to difficulties in regulating menstrual cycles, and both conditions have been linked to an increased risk of developing certain health problems, such as cardiovascular disease.
Summing Up
In conclusion, the connection between Polycystic Ovary Syndrome (PCOS) and Diabetes is a complex one, with both conditions having similar symptoms and underlying causes.
Understanding this link is important for women who are struggling with either condition, as it may help to improve their overall health and prevent the development of serious health complications in the future.
You can consult an OB-GYN or a doctor online through our platform and even enrol in PCOS care plans if you’re suffering from it. Also, if you have any doubts, please feel free to drop them in the comment section.
Leave a Comment
Blogs
Popular Posts
Get the latest from Newmi
Subscribe to get Email Updates!
Thanks for subscribe.
Your response has been recorded.
COPYRIGHT © 2023 KA HEALTHCARE PVT LTD - ALL RIGHTS RESERVED.
Disclaimer: NEWMI CARE does not cater to any medical/Pregnancy or psychiatric emergencies. If you are in a life-threatening situation, please do NOT use this site. If you are feeling suicidal, we recommend you call a suicide prevention helpline or go to your nearest hospital.

0 Comment